Berkeley Talks transcript: Nobel laureate Randy Schekman on new Parkinson’s research
October 4, 2019
Intro: This is Berkeley Talks, a Berkeley News podcast that features lectures and conversations that happen at UC Berkeley. Find more talks at news.berkeley.edu/podcasts, and you can subscribe on Apple Podcasts or wherever you listen.
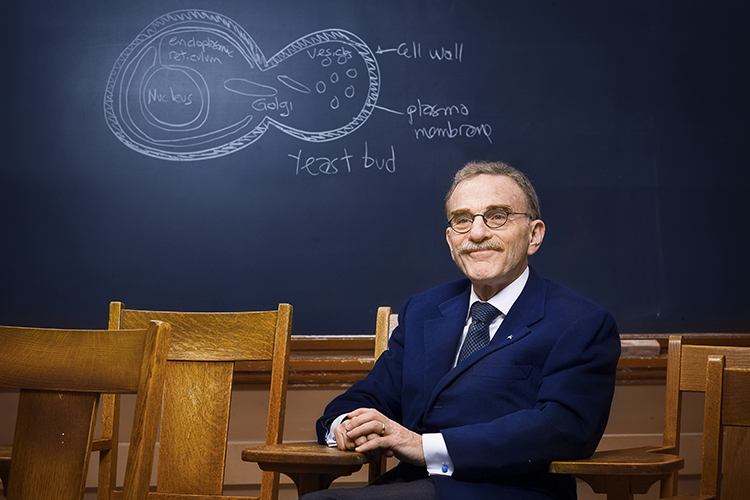
George Brooks: Randy Wayne Schekman was born in Saint Paul, Minnesota. In his youth, his family moved to Orange County. He received a bachelor’s in electrical sciences from the University of California, Los Angeles, and his PhD from Stanford university. After joining the faculty at Berkeley, he was promoted to associate professor and then full professor in 1994. Since 1991, Schekman has been Howard Hughes Medical Institute investigator. His current position is in the Division of Biochemistry and Molecular Biology, Department of Molecular and Cell Biology here at Berkeley. His lab is world famous. He has won numerous awards in biology and medicine. But I think most prominent was the fact in 2013 he was awarded a Nobel Prize in physiology or medicine.
Among the many various accolades one could be bestow on our next speaker, it’s important to recognize that he’s a supporter of Berkeley. For instance, he’s here today. So ladies and gentlemen, it’s my pleasure to give this podium over to Professor Randy Schekman. His keynote is titled “The Challenge of Unraveling the Basis of Parkinson’s Disease.” Ladies and gentlemen, Dr. Schekman.
Randy Schekman: Thank you, George. Thank you, David. And good afternoon. I’m going to tell you about an area that is new to me scientifically, but which I am deeply involved in, and that is to organize a basic research effort that will, we hope, help in identifying the origin and means of progression of Parkinson’s disease. Let me start by reminding you what you heard this morning from some of the first speakers, and that is that human health has been greatly affected by terrible diseases, cancer, heart disease, but tremendous progress has been made in these areas.
In heart disease, we have drug treatments, we have surgical procedures that have greatly reduced the incidents of death that’s brought about by heart disease. And in cancer, we have drugs and immunotherapy. You may know that one of our great, unfortunately former colleagues, Jim Allison, was the one who invented immunotherapy, which is now credited with curing many forms of cancer. But what is overwhelming the population going forward is the incidence of neurodegenerative disease, and I’m going to tell you specifically about Parkinson’s disease. So let’s see if this thing works for me.
We have experienced a pandemic in Parkinson’s disease. The incidence, as you’ll see is increasing dramatically in spite of the fact that the disease was first recognized and reported by clinical symptoms now 200 years ago. As the population inexorably ages, we are experiencing a wave of this disease which inexorably takes the lives of those who are afflicted. Here is a plot of the current incidence of the disease. There are now a million patients afflicted with Parkinson’s disease in the United States, but overwhelmingly, the disease is of international distribution, as you’ll see in the next slide. The disease will affect China disproportionately. Over half of the incidence of the diseases expected to affect China by the year 2030.
Now, one of the problems in defining the disease is it’s limited to symptoms, to the behavior, movement, disorder or the dementia that accompanies 30% of the disease. But there are no biological markers. There is nothing that can be used other than this physical symptom and cognitive recognition to mark individuals who have this disease. So unlike with Alzheimer’s where there are at least noninvasive probes have amyloid plaques, there is nothing for Parkinson’s disease. So as a consequence, the disease has a spectrum of pathology and so it may be more like autism than like an individual disease. It may be more like cancer where there are hundreds of different types of cancer.
There are patients who are diagnosed very early. Michael J. Fox was diagnosed with Parkinson’s disease in his 30s. Often, but not always, these patients suffer an early demise, they have dementia or on the other extreme, the more common late onset form the disease can lead to longer survival, little dementia, but nonetheless, the inexorable progression of the disease. As a result of this range of pathologies that are lumped together as Parkinson’s disease, the drugs that have been tested and developed in an attempt to cure the disease have been largely unsuccessful.
So you’ll see on the left a number of clinical trials for drugs that ultimately have failed. The only treatments for the disease mitigate some of the physical symptoms. Patients who have a movement disorder or a tremor are treated with a substitute for dopamine, the neurotransmitter that is lost progressively as patients succumb to the disease. More recently, there’s an intervention, a surgical intervention called deep brain stimulation, which also limits some of the physical disabilities, but these treatments, the treatment with dopamine or deep brain stimulation do nothing to arrest the inexorable progression of the disease. There continue to be drugs in the pipeline, as you see on the right. There is always hope, but the problem is that there are no ways to evaluate other than the symptoms. There are no ways to evaluate biologically what may happen as the disease progresses.
So let’s have a little bit of the basis of the disease. Let’s look here at a section through a brain. If you look on the left, you’ll see two images. The one labeled P is a brain section from a normal patient and for contrast, look at the section on the right labeled C. That is a normal patient. You’ll see a little band. If you look, this looks kind of like a hat. If you look about the rim of the band in sample C, you’ll see a dark staining region. This is the region of the brain that’s referred to as the substantia nigra. It is the location of some tens of thousands of nerve cells that are busy making the neurotransmitter dopamine.
Dopamine is involved in controlling movement. It’s involved in many other responses, many other neural pathways such as executive function and patients who develop the motor symptoms have, as you heard this morning, already have lost the majority of these cells. These cells stained darkly because they produce a substance called melanin, a natural product that is a reflection of one of the biochemical pathways in these cells. So you see on the specimen on the left that such cells have largely disappeared in these patients and so thus the disease.
Now, more recently, but still quite a long time ago, on close inspection of this region of the brain called the substantial nigra, pathologists were able to notice an inclusion often found within the dopaminergic neurons. You see on the right, this is an electron micrograph of a region of the brain containing these cells and you see at the bottom of this a kind of a disk shaped dark object which has been referred to as a Lewy body first found now over a hundred years ago by a pathologist by the name of Frederick Lewy. It is often found but only can be detected in biopsies of patients who have died and who’ve had their brains dissected.
Most recently, you’ll recall the sad story of the comedian Robin Williams, who suffered from dementia and various forms of panic disorder was diagnosed as a form of Parkinson’s disease, but he regrettably then committed suicide because he was so distraught. His wife, Susan, had his brain dissected and they discovered these Lewy bodies all over the brain, not simply restricted to the substantia nigra. There was an enrichment of these Lewy bodies in the amygdala, and in his case, he had panic disorder as a result of this disease.
Now, this is a marker that is seen in the brains of patients who are deceased, but there is no way of probing the existence or presence of the Lewy body until a patient’s comes. There are no noninvasive probes that we have yet to be able to diagnose the presence of this element of the pathology. Of course, mindful of the experience with Alzheimer’s disease and the plaques that you heard about this morning, one must be cautious about interpreting whether these Lewy bodies really are the basis of the disease or merely some byproduct of some unfavorable neural network. That remains a question for future investigation.
Now, still focused on that one issue, there is a theory that is indicated here in this section. It’s a cartoon of a brain that shows these Lewy bodies and you see these yellow little dots progressing from the base of the brain and then spreading throughout the brain. There is a view, again, not substantiated by any particular experimental evidence, that these Lewy bodies may be produced very early on at the base of the brain and then move laterally within the brain over the decades that a patient suffers from this disease.
Now more recently, it’s been possible to take the protein that is the basis of Lewy bodies. It’s a protein called alpha synuclein. It’s a protein that’s found in brain cells. This protein is enriched in the Lewy bodies. It’s possible to take this protein in the laboratory and make aggregates of the protein and then inject them into the brain of an experimental animal. And you see here in two research publications that when that is done, one can detect within the animal brain the spread of these Lewy bodies to different regions. It’s even more recently been possible to introduce these aggregates of synuclein into the gut of an experimental animal and within months, these Lewy bodies spread from the gut into the brain and throughout the brain.
Now, the problem is that again, there is no real notion yet whether the Lewy body is the basis of the disease and furthermore, there are really no good experimental animals that matched the progression of the symptoms of the disease as seen in the human patient. So this is the problem that we face in trying to understand how this disease originates and progresses. Still a lot of ignorance.
Now, let me tell you about a new effort that I’ve become involved in. My research does not involve evaluating Parkinson’s disease, but I have been personally affected by this. My wife suffered for 20 years from Parkinson’s disease and died as a result of that two years ago. Around that time, I was approached by a representative of the Sergey Brin Family Foundation. Mr. Brin, the cofounder of Google, has a family history of Parkinson’s. His mother has a genetic form of the disease and he has inherited one copy of the mutant gene from her and because of the nature of this mutation, he is at some risk.
As a result, he has invested quite a considerable sum in research supported by the Michael J. Fox Foundation, one of the major organizations to support Parkinson’s disease, but he decided because most of that work by that foundation and much of the work supported by the NIH is oriented to the clinic, that what we really need is more of a basic research emphasis to understand potentially at a molecular level exactly what goes wrong as patients present with the symptoms. And so as a result, he decided to invest another considerable sum, and I was asked to lead this effort and as a result of my personal involvement, of course I was really quite excited to do so.
And so let me tell you in just a few minutes what we plan to do. We’re launching very quickly, very soon. There’ll be a research article that’s published in a journal called eLife next week that you can look up if you’re interested. It’s an open-access journal, so you’ll be able to have access to that article and see exactly what we’re doing. But let me summarize for you what the plan is.
Again, to emphasize, we want to know where the disease begins, what the molecules and cells and neural circuits are that are affected primarily by the disease and then how it progresses. We do not come into this with any particular bias except the knowledge that about 30% of the disease has a genetic origin, and since they are genes, and those genes have protein products, those are clues that we hope will allow us to understand the basis of the disease.
Now, much of the research that’s gone on in the clinic has been valuable and important, but there are no cures. And so many of us, me being a basic scientist and this fellow named Dario Alessi, likewise, many of us feel that what we really need to do is get into the laboratory to understand these basic processes. And funding bodies, unfortunately, very often ask investigators like me to solve diseases and work with companies to figure out how this may be achieved and made it into a drug. But as I’ve said, and what this fellow also says, we don’t have the fundamental knowledge on which to base these discoveries. So again, the effort will be focused on basic science.
It’s a puzzle. There are many different pieces that come from the genetics that have identified nearly 20 genes. From this puzzle, you can see that some of the genes that have been affected and discovered affect the function and survival of mitochondria, the energy powerhouses of ourselves. Some of the genes affect the process of protein degradation in an organelle called the lysosomes. Some of them potentiate the process of cell death in these cells prematurely. We don’t understand how that is. There are connections between the immune system and nerve cells that are just emerging, but we don’t know what role they may play in how this disease progresses.
So here now are the goals, the particular goals that we have set for ourselves. We will invest in people, investigators, who are studying the genes and the protein products of these genes and the pathways in which these proteins interact that are in normal cells and that go bad in dopaminergic neurons. We will invest in people who are interested in the immune system and the regulation of nerve cell survivability as in relation to the nerve system. There are cells within the brain that are part of a brain specific immune response. They may play a role in the initiation or progression of this disease. We will invest in people who are exploring the circuitry that connect dopaminergic neurons that allow them to develop and that sustain in the normal life. And we will invest in people who are exploring the very early stages before the pathology emerges.
As you heard this morning, there was a very long so-called prodromal phase, sometimes 20 years before a patient experiences the usual movement aspects of the disease where symptoms arise that cannot readily be explained as Parkinson’s. Let me give you two examples. Patients often report that they have a poorly developed sense of smell, sometimes 20 or more years before the pathology clearly emerges. Now, that’s not diagnostic. There are many people who have a poorly developed sense of smell, but a lot of them who then develop Parkinson’s report early symptoms.
Even more unusually, there is another symptom called REM sleep disorder where people who don’t yet appear to have the pathology flail around in their sleep because they live out, they attempt to live out their dreams or nightmares, and this can often be harmful to themselves or to their partners. So REM sleep disorder, what does that have to do with the progression or the development of this disease, which can happen in 10 or more years later? So we want to invest in that.
More specifically, we have the following objectives in the teams that we wish to recruit to our effort. We’re going to look specifically for investigators who are working on interesting problems but who have already assembled a collaborative team of investigators from around the world who know how to work together productively in a team effort. One problem with academic science is the reward structure for an academic scientist typically favors the individual, how that person progresses, how he or she develops his own personal team, but what really works very well with a complicated problem like Parkinson’s is is to bring people together in collaborations, hopefully of an international flavor.
We want to attract people from outside of Parkinson’s, as well as those from within, and we want to attract early career investigators who have not yet experienced the pleasures of working in a collaborative spirit. We’re going to focus on the themes that I presented in the last slide and we’re going to specifically embrace openness. We want to develop an international network of people who are in active communication with each other, who post their work in publicly accessible databases, who post their publications on a preprint server and who publish in open-access journals so that everyone, not just those associated with an academic community, will have access to the work to follow what we’re doing.
So stay tuned. Next week, we will publish our first article in the journal eLife, a website that you can look up called “ASAP Parkinson’s.” If you just Google “ASAP Parkinson’s,” you’ll see the outline of the plan. It will appear in a new form next week and at the end of the year, we will start receiving applications for this funding from investigators from around the world. The challenge is great, but the resources from Mr. Brin are really quite substantial and the will is there to make progress on this deadly disease. Thank you.